Breast cancer is the most common cancer among women in the United States and the second leading cause of cancer death among women behind lung cancer. One in 8 women will develop breast cancer in their lifetime.
Today there are over 2.6 million breast cancer survivors in the United States. Public awareness of the disease and greater efforts for early detection with screening mammography have increased early detection of the disease, treatment and long-term survival. Early stage localized breast disease is associated with a 98% 5-year survival rate.
Before & After
View More

The Consult
Your initial consultation will take approximately one hour. During this time, Dr. Liu will take a thorough medical and breast history, help you with the decision making process, and answer all of your questions. Dr. Liu understands the importance of your oncologic treatment plan as the centerpiece in planning the appropriate reconstruction. The goal of the consultation is for you to obtain all the information you need to make an informed decision regarding the different types of breast reconstruction (implant vs. autologous) and to determine which method is best for you.
Schedule a Consultation

About the Operation
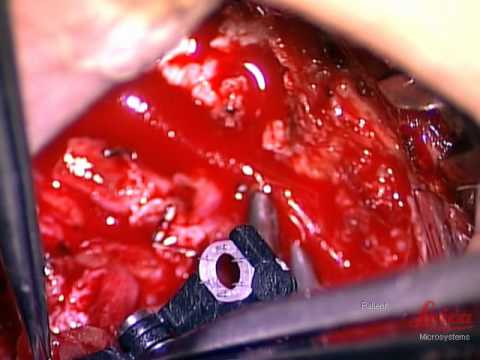
Breast reconstruction typically takes 3 stages (operations) to complete. Whether you choose implant or autologous reconstruction your initial breast reconstruction (Stage 1) will be performed at one of the hospitals we are credentialed at. For immediate reconstructions, the plastic surgeon(s) will work closely with the surgical oncologist for optimal safety and aesthetic results. The reconstruction can be performed immediately after or at the same time as the breast surgery. For delayed reconstructions, the surgery is performed entirely by the plastic surgeon(s). After your recovery (typically 3 months) you will proceed with the second stage of your reconstruction (Stage 2). The goal of the second stage is to shape and size the breast to it final form. In the case of a unilateral reconstruction, the reconstructed breast is made to replicate your native breast. Sometimes, the uninvolved breast will need to be lifted, reduced, or augmented to match the size and shape of the reconstructed breast, also known as the symmetry operation. For implant reconstructions, the tissue expander is exchanged for a final silicone implant at the second stage.
Unfavorable scars are also revised at this time and excess subcutaneous tissue can be removed via liposuction. Although these procedures are “cosmetic” in nature, these symmetry procedures are an integral part of the reconstruction and are fully covered by insurance as mandated by the Women’s Health and Cancer Rights Act of 1998. These procedures are done in an outpatient surgery facility and you will be discharged home after the procedure.
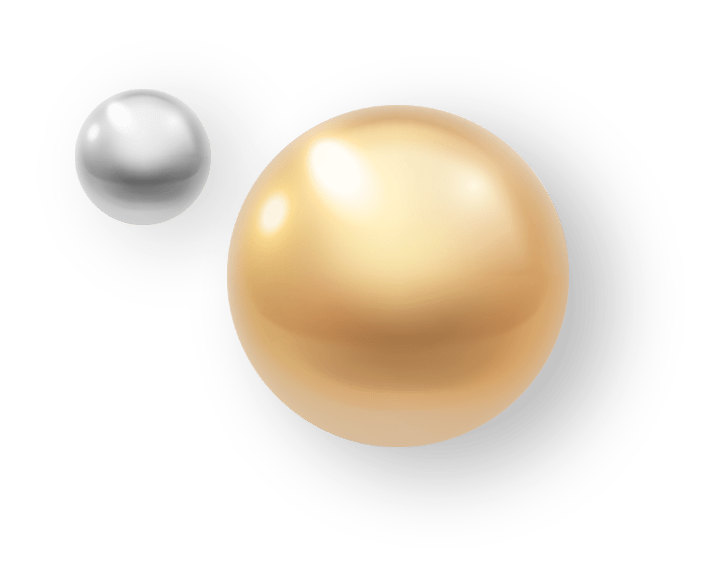
Once the breast shape and size are finalized, the nipple is reconstructed (Stage 3). The nipple-areola complex (NAC) reconstruction (Stage 3 and 4) are the final steps of the reconstruction and are not performed until the final breast shape and size is achieved. The NAC is considered the crown or peak of the breast and is reserved until the final breast shape and size is achieved. This procedure is performed as an outpatient and can usually be done under local anesthesia. Once the nipple reconstruction fully heals the areola is tattooed.